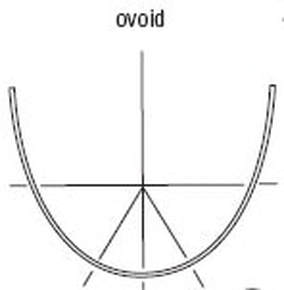
 The question is, what should we do when we can’t have both, beautiful alignment AND occlusion? Why can’t we always have both? Simply because the teeth in a human body don’t work like the teeth on a wax typodont or a plaster model. Neither can the occlusion be changed as it can on models, by trimming the models, nor can the teeth necessarily be put into what we consider “ideal” alignment, as identified, for example, by the American Board of Orthodontics parameters for “ideal.” “Wha??," you ask. Ovoid arch forms Ovoid arch forms, which, according to Ricketts, are found in 25 percent of the population, do not align to meet ABO criteria due to the greater curvatures and resulting positions of the teeth in alignment. In an article by Kazuhito, A., and Will, L., the ovoid arch form is shown to be the arch form having the greatest variations among the examiners who are ranking them. (https://doi.org/10.1016/j.ajodo.2009.12.032) Second molar prematurities This may be the most common reason to consider carefully before bracketing 7’s. Second molars have a good chance of extrusion, when included in the archwire. And, if they extrude, voila! an iatrogenic prematurity, iatrogenic CR-CO discrepancy, and a risk introduced for future dysfunctional occlusion, need for RCT on a tooth that takes a pounding (and has no decay). We never want our orthodontic treatment to contribute to dysfunctional occlusion. Here’s the real problem; the variable human body and variable tooth responses. Each body acts and reacts differently. Some folks can eat carbs/sugars all day and not get fat. Some cannot. Some people smoke and live to be 100 years old. Most do not. Why? Some people can have a CR-CO slide and never have a symptom or problem. Many people have symptoms - craniofacial, neck and back pain, fractured molars, non-carious, non-vital molars needing RCT, gingival margin recession, especially in bi’s and molars and in the absence of perio disease, posterior crowns, abfractions, worn occlusal surfaces of posterior teeth? Each human body reacts differently. And, adults are often not very adaptable. Our orthodontic treatment – mechanics – must be considered at risk of being etiologic (iatrogenically) in occlusal dysfunction. So where does this leave us with those blessed second molars? It leaves us with a strong and careful consideration if they should be bracketed, or not. It just may be that the occlusion may be better without putting the 7’s into “harm’s way.” Even rotated, or malposed, are they quietly ok in the occlusion? A patient may have MANY “CO” bites. Some patients are all over the map with their comfortable or uncomfortable bite. And some patients’ musculature and resulting joint movements will change the bite with the tiniest - and I do mean TINY - changes, like a new restoration with even tiny high spot. Consider that we never really know where a patient’s functional AND dysfunctional occlusion will be next. Keep that in mind when you consider bracketing those most-likely-to-extrude-7’s. Which brings us to another reason not to bracket teeth: The patient presents with signs and symptoms of dysfunctional occlusion. Perhaps minor treatment, anterior alignment, with anchored posteriors is a consideration. Perhaps NO orthodontic treatment is the right choice. Neither you nor your patient want the situation to be worsened. Don’t bracket a tooth just because it’s white.
0 Comments
Leave a Reply. |
Dr Chris BakerAmerica's most-trusted teacher of orthodontic continuing education, Dr. Chris Baker has practiced and taught for more than 30 years, and is a current or former faculty member of three U.S. dental schools. She is a pediatric dentist, author, blogger, dental practice consultant, and mentor. Dr. Chris is also Past President and Senior Instructor of the American Orthodontic Society. She is based in Texas, USA, but lectures around the world. Categories
All
Archives
July 2024
Text and images
© 2024 Dr Chris Baker |



 RSS Feed
RSS Feed